

Simple, Automatic,
Powerful:
With COMP+, you are in control.
OnePoint Patient Care’s COMP+® is your responsive PBM partner, offering the industry’s most advanced and intuitive web application for medication management of your workers’ comp claims.
With COMP+®, our technology-enabled and intuitive PBM platform, high-touch account management and Claims Manager support makes it simple for your staff to work efficiently and control costs automatically with medication utilization management. Our proprietary technology is built based on decades of integrated pharmacy and PBM experience. We give your claims adjustors everything they need to stay compliant, control costs – and get injured worker’s back on their feet as soon as possible.
COMP+ partners are free to choose how to manage claims, including setting medication cost thresholds, automatically approving medications, and setting clinical intervention rejections with parameters such as day supply, quantity and many more. Manage the medication side of claims with the philosophy you believe in.*
COMP+ is a lean and flexible PBM and application service offering, with transparent pricing models, customizable clinical reporting, pharmacy search, rebates aggregation and full compliance support – giving your organization everything you need (and nothing you don’t) with the ability to scale. We provide you with insightful, actionable data – not just standard reports – that is based on what matters to your organization, including early identification and real time updates, that will help drive informed decision making throughout the life of a claim.
COMP+ offers your staff best-in-class customer service, including dedicated pharmacist consulting. Put our experience and our reputation to work for you and your patients.
Contact Us to learn more about COMP+
Benefits of the COMP+ Application
- COMP+ is a lean and flexible PBM and application service offering, with transparent pricing models, customizable clinical reporting, pharmacy search, rebates aggregation and full compliance support – giving your organization everything you need (and nothing you don’t) with the ability to scale.
- We provide you with insightful, actionable data – not just standard reports – that is based on what matters to your organization, including early identification and real time updates, that will help drive informed decision making throughout the life of a claim.
- COMP+ empowers your Claims team to manage the entire medication benefit of a claim, creating efficiencies and ensuring cost-savings.
- 24/7 access to our support staff as well as a Worker’s Compensation dedicated pharmacist, and backed by OnePoint Patient Care, an industry leader in high-touch pharmacy and PBM service.
- Claims adjusters can easily make coverage decisions in real time that affect the outcome of patient care directly at the pharmacy counter.
HOMEPAGE
- Immediately upon logging into Comp+, Claims Managers have an overview of open and important Tasks that result in efficient/effective care to the injured worker
- Claims Managers can quickly and easily navigate to their important tasks and make decisions in real-time
CLAIM SCREEN
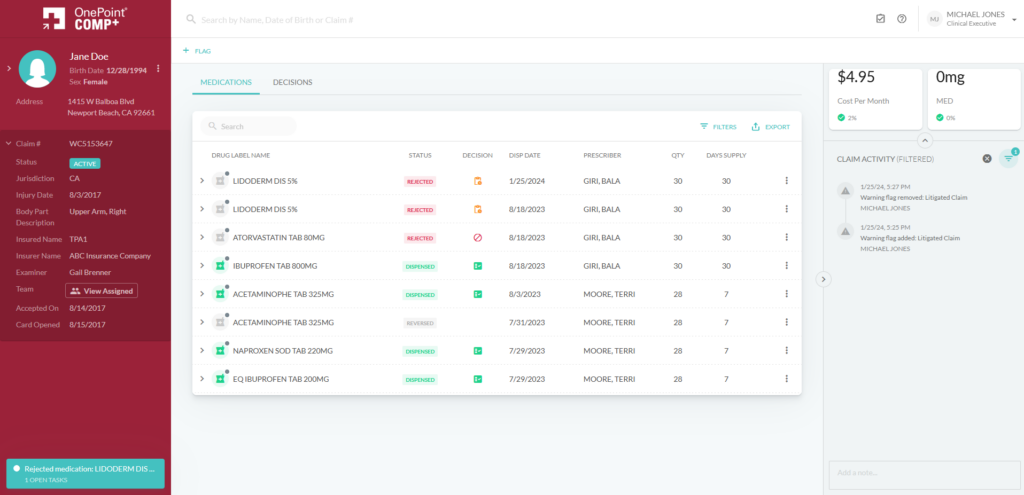
- View the patient’s entire claim history, all in one convenient place and allow for exportation of claims data for legal settlement
- The functionality provided in the application specifically allows the adjuster/examiner to make informed decisions in real-time on the proper medications related to the injury
- Managers have oversight over the entire medication history of their patient’s injury claim, with all Activity visible in a comprehensive and filterable timeline
Flagged Claim Screen
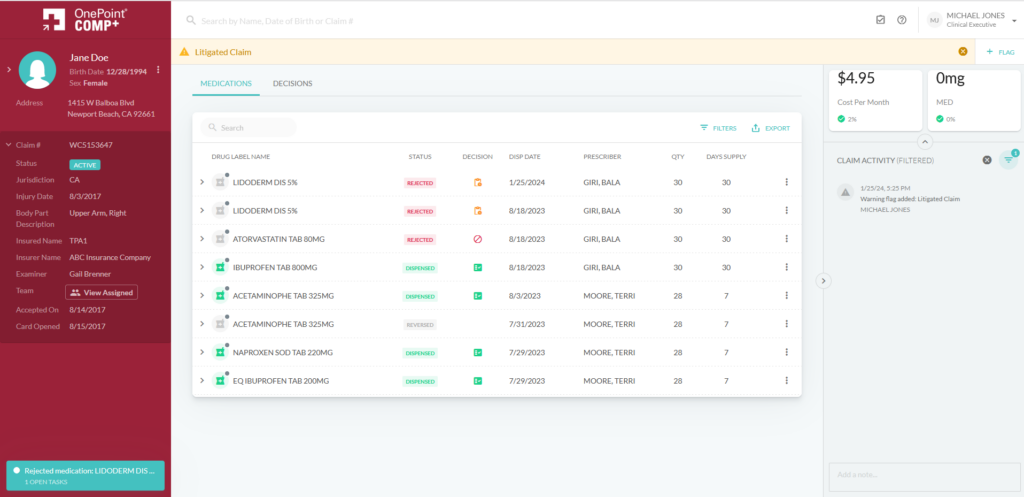
- Manager can review the status of their patient’s claim, including the reason for the decision whether a prescription was Blocked, is Still Pending, or has been approved
- When a prescription is selected, the Claims Manager can see exactly what the cost for the mediation will be (estimate) and the exact total amount once the claim is processed
- Notes/Flags in the system allow cross user communication on the status of a claim and special annotations that help manage the claim more effectively
Decision Tab
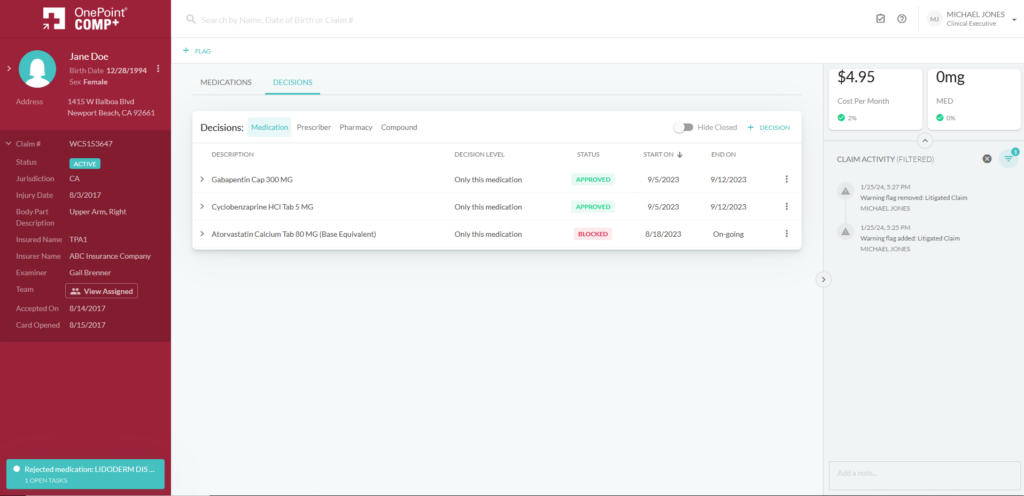
- Here your managers can quickly and easily review the decisions made throughout the life of a Claim, broken out by Type (Medication, Prescriber, Pharmacy) and Compound decisions
- This helps users understand the progression of the medication claim coverage decisions
COMP+ empowers your Claims team to manage the entire medication benefit of a claim, creating efficiencies and ensuring cost-savings.
- Empower your Claims Team: to make informed decisions about what is best for the patient, every step of the way.
- Save money: with transparent and flexible pricing models, and instantaneous access to pharmacy and claims data.
- Enjoy best-in-class customer service: with 24/7 access to our support staff as well as a Worker’s Compensation dedicated pharmacist, and backed by OnePoint Patient Care, an industry leader in high-touch pharmacy and PBM service.
Contact Us to learn more about COMP+
*All medication and pricing limitations must meet all state and federal regulations.
Network Pharmacy Locations
Hospice providers, caregivers, and injured workers can find the closest pharmacy partner in our contract partner network.
State Formularies
Prescribers looking for COMP+ administered worker’s compensation formularies can find all current documents here.
Mail-Order Enrollment Process
Injured Workers with medication benefits administered by Comp+ and looking for a mail order option.
State Formularies

